取穴部位:第4後仙骨孔部
筋肉:仙棘筋
運動神経:脊髄神経後枝
知覚神経:中殿皮神経
血管:外側仙骨動脈
BL34 下髎(げりょう)
基本情報
- 経絡:足の太陽膀胱経
- 穴性:阿是穴、八髎穴の一つ
- 部位番号:BL34
名称の由来
「下」は下方を、「髎」は骨の孔を意味し、第1~第4後仙骨孔のうち最下方にあたる第4後仙骨孔を指すことから名付けられた。左右に並ぶ4つの後仙骨孔の上から順に上髎・次髎・中髎・下髎と呼び、これらを総称して八髎穴と称する。
取穴部位と取穴法
取穴部位
仙骨部に位置する第4後仙骨孔。
- 後正中線から外方1.5寸に白環兪
- 後正中線から外方3寸に膀胱兪
これらと同じ水平面上のもっとも下方の後仙骨孔が下髎である。
取穴法
伏臥位または側臥位で屈曲位をとらせ、触診で第4後仙骨孔を確認し、その孔内または周縁に取る。
刺鍼・灸法
- 垂直に直刺し、深さは0.5~1寸(骨に触れない程度)とする。
- 刺入後、適宜補瀉を行い、15~20分間置鍼。
- 灸法では、温灸を1壮~3壮行う。
局所解剖
- 組織:皮膚→皮下組織→腰背腱膜→多裂筋(起立筋群)→第4後仙骨孔
- 動静脈:外側仙骨動脈・静脈
- 神経:第4仙骨神経後枝および仙骨神経叢の枝
主な効能・適応
上記の適応は臓器に近い位置にあることから、泌尿・生殖器系疾患の治療にとくに用いられる。
臨床応用例
- 排尿障害:BL34への刺鍼で膀胱括約筋の緊張緩和と尿流改善を報告
- 月経痛:BL34とBL32の併用により子宮収縮抑制と鎮痛効果
- 坐骨神経痛:BL34を中心にBL32~BL36群で仙骨周囲の血流促進
- 産後ケア:会陰部疼痛緩和および子宮復古促進
一部症例報告で、BL34刺激による排尿パターンの正常化や疼痛スコアの有意改善が示唆されている。
参考文献
- 長瀬善夫, 東洋医学概論, 創元社 (1961) 編著者ら. 「ツボ辞典 BL34.下髎(げりょう)」
- TSUBOLAB®. 「下髎(げりょう)[BL34]」
- 東洋医学系総合サイト Higokoro. 「足の太陽膀胱経のツボ一覧」
今後はBL32やBL35との連携刺鍼、八髎穴全体を用いた産科・整形外科領域の併用法、また近年の超音波ガイド下刺鍼の安全性検証なども追ってみると、さらに臨床応用の幅が広がります。
Related Acupuncture Points for BL34(下髎)
八髎穴(Sacral Foramina Points)
|
|
|
|
これらはすべて後仙骨孔を通る同じ部位のツボで、排尿・生殖器系や会陰部の疼痛改善に併用されます。
近位の局所ツボ
- 白環兪 BL30(後正中線外1.5寸、BL34と同じ水平面)
- 会陽 BL35(肛門外側1寸、会陰部の痛みに有効)
- 環跳 GB30(大腿外側の最大隆起部、坐骨神経痛に併用)
前募穴・背兪穴の併用例
- 中極 CV3(下腹部の膀胱・尿道症状に)
- 関元 CV4(生殖器系の調整に)
- 膀胱兪 BL28(泌尿器系全般のバックアップ)
- 三焦兪 BL22(下焦の気機を整える)
臨床でのコンビネーション例
- 月経痛:BL32+BL34+BL33
- 排尿障害:BL28+BL30+BL34
- 坐骨神経痛:GB30+BL36+BL34+BL37
- 会陰部疼痛:BL34+BL35+CV3
これらの組み合わせは、患部への局所的な刺激と経絡全体の流れを同時に調整することで、相乗効果を高めます。
How These Points Are Used in Treatment
To address pelvic, urinary, reproductive, and low-back conditions, practitioners select and combine BL34 with related points based on syndrome differentiation. Needling techniques, depth, manipulation, and adjunct therapies (moxibustion, electroacupuncture) are tailored to each patient’s presentation and treatment goal.
1. Syndrome Differentiation and Point Selection
- Urinary Dysfunction (滞尿、頻尿)
• Primary: BL28, BL30, BL34
• Supplementary: CV3 for bladder control, CV4 for tonification - Menstrual and Gynecological Disorders (月経痛、不妊)
• Primary: BL32, BL33, BL34
• Supplementary: CV3 for uterine regulation, SP6 for blood circulation - Sciatica and Low-Back Pain (坐骨神経痛、腰痛)
• Primary: GB30, BL34, BL36
• Supplementary: BL37 to extend analgesic zone, BL40 as distal point - Perineal and Postpartum Pain (会陰部疼痛、産後ケア)
• Primary: BL34, BL35
• Supplementary: CV1 for lower-jiao regulation, DU1 for perineal circulation
2. Needling Techniques and Parameters
3. Protocols for Common Conditions
- Urinary Retention
- Points: BL28, BL30, BL34, CV3
- Method: Prone needling on bladder line, then supine for CV3; combine with warm moxa on CV3.
- Frequency: 2–3 sessions per week, total 6–8 treatments.
- Dysmenorrhea
- Points: BL32, BL33, BL34, SP6
- Method: Electroacupuncture at BL32–BL34 (2 Hz), manual tonification on SP6.
- Frequency: 1 session before menstruation, 2 sessions during pain peaks.
- Sciatica
- Points: GB30, BL34, BL36, BL37
- Method: Perpendicular needling at BL34 and BL36; GB30 with strong lifting-thrusting; BL37 lightly tonifying.
- Adjunct: Cupping along the sciatic pathway.
- Frequency: 2 sessions per week for 4 weeks.
- Postpartum Perineal Pain
- Points: BL34, BL35, CV1, DU1
- Method: Lateral position for BL34/BL35; supine needling for CV1; mild even manipulation.
- Adjunct: Warm moxa on DU1.
- Frequency: Daily for 5 days, then every other day for 2 weeks.
4. Clinical Considerations
- Always confirm absence of sacral fractures or skin lesions before needling posterior sacrum.
- Use sterile, single-use needles and maintain proper hygiene.
- Monitor patient comfort—sacral region can be sensitive; adjust depth accordingly.
- For patients on anticoagulants, apply minimal manipulation and shorter retention.
- Document response each session and modify point selection based on progress.
5. Beyond Manual Needling
- Ultrasound-Guided Acupuncture: Enhances precision around sacral foramina, reduces risk of nerve stimulation.
- Agent-Based Modeling (ABM) of Acupuncture: Simulates local tissue response, optimizing point combinations virtually before clinical trials.
- Integrative Protocols: Combining pelvic floor physiotherapy with BL34 electroacupuncture for refractory urinary incontinence.
For further exploration, consider recent studies on sacral foramina needling under real-time imaging and emerging insights into neuromodulation effects via low-frequency stimulation.
Importance of Needling Techniques
Needling techniques are pivotal in acupuncture because they determine the specificity, safety, and magnitude of therapeutic effects. Precise control over angle, depth, manipulation, and retention time allows clinicians to target distinct neural and fascial pathways, modulate local blood flow, and optimize patient comfort.
1. Precision and Safety
Accurate needle placement minimizes risk and maximizes efficacy:
- Anatomical accuracy
• Ensures needles avoid major vessels, nerves, and organs
• Targets the intended myofascial or neurovascular bundle - Depth control
• Superficial vs. deep insertion engages different receptors (cutaneous vs. proprioceptive)
• Prevents puncture of organs or bony contact - Angle of insertion
• Perpendicular for focal stimulation of deep foramen (e.g., BL34)
• Oblique or transverse to skirt sensitive structures and broaden the stimulation zone
2. Mechanistic Rationale
Different needling manipulations elicit distinct physiological cascades:
- Neuro-modulation
• Lifting-thrusting and rotation activate Aδ and C fibers, triggering endorphin release
• Low-frequency stimulation (2 Hz) enhances enkephalin and β-endorphin pathways - Mechanotransduction
• Needle rotation winds collagen fibers, generating fibroblast signaling and local cytokine changes
• Promotes microcirculatory improvements and tissue remodeling - Inflammatory modulation
• Microtrauma from needling up-regulates anti-inflammatory mediators (IL-10, TGF-β)
• Balances pro- and anti-inflammatory cytokines in chronic pain
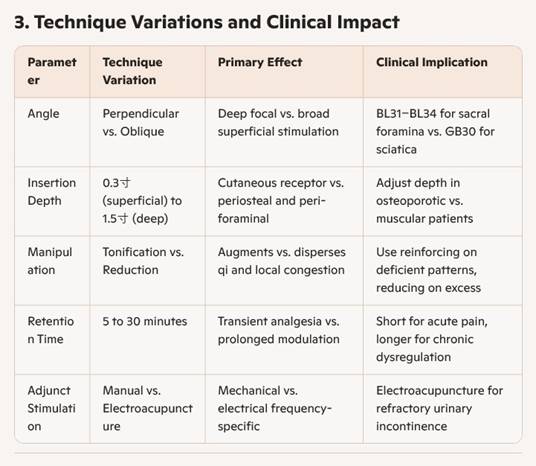
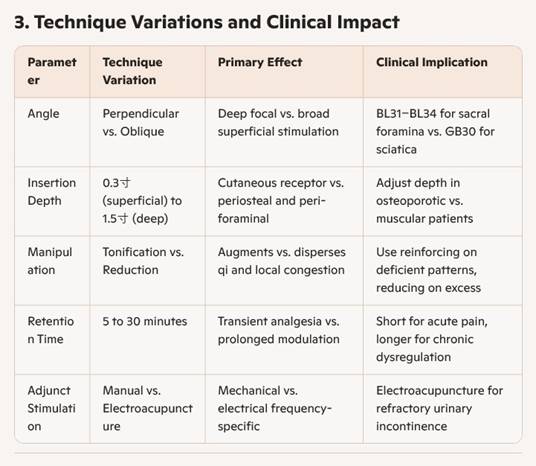
3. Technique Variations and Clinical Impact
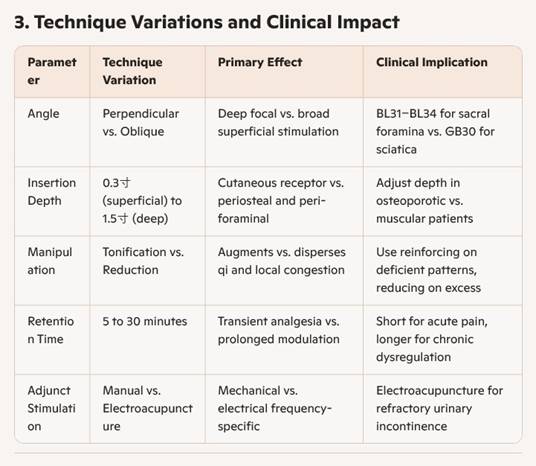
4. Integration with Advanced Modalities
- Ultrasound Guidance
• Real-time visualization of sacral foramina and nociceptive tissue
• Enhances accuracy in deep points like BL34, reducing inadvertent nerve contact - Electroacupuncture
• Delivers controlled frequency and intensity to amplify neuromodulation
• Custom programs (2 Hz/100 Hz alternating) for mixed pain syndromes - Agent-Based Modeling (ABM)
• Simulates local tissue and immune response to different needle manipulations
• Optimizes point combinations and parameters before clinical trials
5. Training, Standardization, and Quality Assurance
Consistent outcomes depend on rigorous practitioner education and protocol standardization:
- Hands-on workshops with anatomical cadaver models
- Standard operating procedures for point location, needle handling, and hygiene
- Regular skills assessment and peer review
- Integration of patient-reported outcome measures to refine technique
For deeper exploration, you may consider:
- Investigating the role of needle material conductivity on electrical stimulation efficacy
- Reviewing studies on cytokine profiles post-acupuncture needling
- Exploring smartphone-mounted sensors that quantify needle vibration and tissue resistance
- Examining protocols for hybrid therapies combining manual therapy and ultrasound-guided acupuncture
Different Needling Techniques
The world of acupuncture offers a variety of needling methods to tailor stimulation to each disorder, tissue type, and treatment goal. Below is an overview of the main techniques:
1. Insertion Angle Techniques
- Perpendicular
Insert the needle at a 90° angle to the skin. Provides focal, deep stimulation—common for points over bony structures like BL34. - Oblique
Angle the needle 15–45° relative to the skin. Allows safer access near sensitive areas or broadens the stimulation field. - Transverse or Subcutaneous
Thread the needle almost parallel to the skin surface. Ideal for points on muscles or fascial planes to mobilize qi superficially.
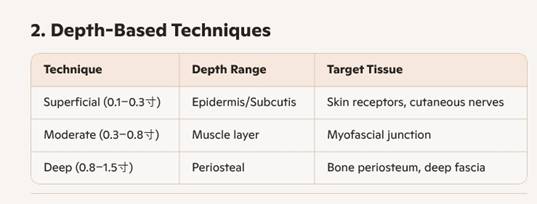
2. Depth-Based Techniques
3. Manual Manipulation Methods
- Lifting-Thrusting
Repeated, gentle vertical movements. Activates mechanoreceptors, ideal for pain relief. - Twisting-Rotation
Rotating the needle clockwise or counterclockwise. Winds collagen fibers, boosting fibroblast signaling. - Pushing-Pulling
Alternating forward/backward pressure without full insertion depth change. Fine-tunes local qi flow. - Even Method
Minimal manipulation after insertion. Suitable when mere presence of the needle suffices (e.g., fragile patients).
4. Reinforcing (Tonification) vs. Reducing (Sedation)
- Tonification (補法)
• Slow insertion, mild lifting-thrusting and rotation, leaving needle in place with gentle “catch.”
• Used for deficiency syndromes or chronic fatigue. - Sedation (瀉法)
• Rapid insertion, strong thrusting and rotation, quick removal or vigorous stimulation.
• Used for excess patterns, acute pain, or inflammatory conditions. - Neutral (平補平瀉)
• Balanced insertion and manipulation.
• Employed when neither clear excess nor deficiency—common in most musculoskeletal complaints.
5. Specialized and Adjunct Techniques
- Fire Needling
Briefly heat the needle before insertion to combine thermal and mechanical stimulation—used for cold–damp conditions and chronic pain. - Warm-Needle Moxibustion
Attach a small moxa cone to the needle handle. Provides sustained heat along the channel. - Electroacupuncture
Clips a low-frequency electrical stimulator to inserted needles. Precise control over frequency and intensity, excellent for refractory pain or urinary disorders. - Intradermal Needles
Tiny needles embedded for hours to days. Maintains mild, continuous stimulation—often used for chronic gynecological or digestive issues. - Plum Blossom (Seven-Star) Hammer
Lightly tap the skin to create multiple micro-punctures. Useful for dermatoses, localized analgesia, or desensitization therapies.
Next-Step Explorations
- Compare local cytokine changes after tonification versus sedation methods.
- Investigate needle conductivity and optimal waveforms in electroacupuncture.
- Explore ultrasound guidance to refine angle and depth in sacral foramen points.
- Simulate needling strategies in agent-based models to predict patient-specific responses.
解剖学的データ
|
筋肉 最大の背筋で、脊柱を伸展して屈曲するのを防ぎ、脊柱を起立させる働きがある。脊柱起立筋はさらに、腸肋筋・最長筋・棘筋の3つに分けられる。 |
|
運動神経 脊髄に出入りする末梢神経のことで、頸神経・胸神経・腰神経・仙骨神経・尾骨神経よりなる。脊髄神経の前枝は後頭部・胸部・腹部・上肢・下枝の筋肉や皮膚を、後枝は肩背部・腰部・臀部の筋肉や皮膚を分節的にする。 |
|
知覚神経 第1~第3仙骨神経の後枝から起こり、殿部の知覚を司る神経。 |
|
血管 内腸骨動脈から分岐する動脈で、第4・5腰神経、第1・2・3仙骨神経の神経線根を栄養する。 |
主治・対象疾患
|
|
|
|
|
|
|
|



